Life continues to improve after a minor scare. My post-treatment scans included a PET scan that “lights up” with certain cells–most notably, cancerous cells. The full-body scan delivered excellent news in that there were no visible signs of cancer anywhere in my body, but there was a small amount of light up at the tumor site. After a lot of arguing between my oncologist (who feared the worst) and my radiologist (who believed the tumor was dead and the minimal light up was a side effect of radiation treatment), the “tumor board” met and concluded that there was no evidence of disease. Yay! In fact, they don’t even see the former tumor in the scans. From a softball to nothing in a year. Moving forward, I will have an MRI of my pelvis and a CT scan of my chest every three months for the next five years. Then it will become an annual set of scans until something else kills me.
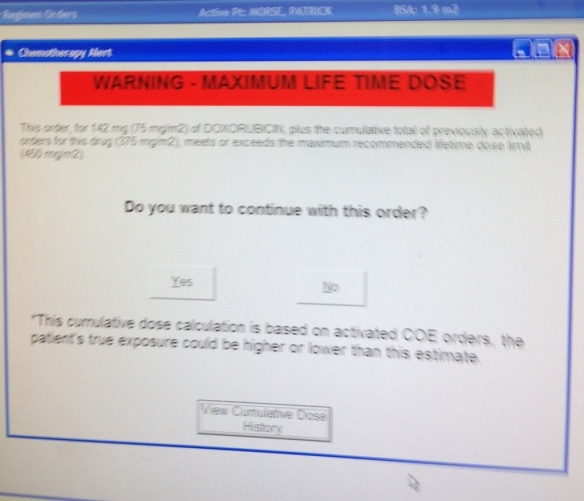
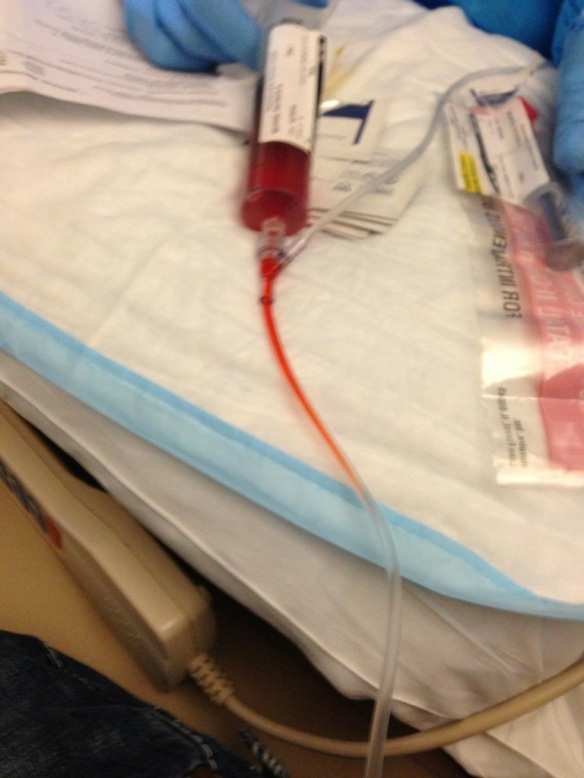
Thanks to the clean scans, I had my port removed. This small device was implanted in my chest, with the tubing going into my jugular. It made the delivery of chemo faster, safer, and easier. Instead of searching for a vein, the needle was put directly into the port. This would break skin, of course, but it would only hurt for a second or two and then be fine for the duration of chemo and fluids (2-5 days of being connected to something. I couldn’t even feel the needle being taken back out. The port could also be used to draw blood, so it was quite useful. Fortunately, I was allowed to keep my port. It was a part of my body for so long, I’m thankful I don’t have to lose it completely. See how cute it looks:
This morning I woke up at 5:20a.m. because all of the great news I’ve been receiving means that it’s back to work for me. The last year has been all about getting me back to doing what I love. Incidentally, today is day 365 in my journey. Tomorrow marks one year since I received the phone call that there was “something” on my MRI. So here I am, taking a selfie while cleaning my classroom.
Four former students also came to help–incidentally, the same students who were cleaning my classroom when that terrible phone call came in last year. To be fair, we were eating lunch when the call came in. We ordered from the same restaurant again today.
After a year of this journey, what have I learned? Enough to know not to share the answer to that question and enough to know that having lunch with those same four students today makes me about the most fortunate person on the planet.